▶ Watch Video: Who is eligible to get the COVID-19 antiviral drug Paxlovid?
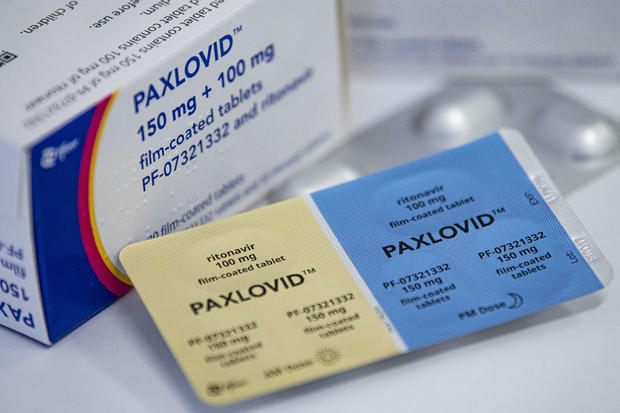
Scientists and federal agencies say they are investigating reports of Americans who say they faced a resurgence of COVID-19 soon after finishing off a course of Paxlovid, Pfizer’s antiviral treatment for the disease.
Often referred to as a “rebound” or “relapse” of COVID-19 after taking the standard five days of Paxlovid pills, experts say key questions need to be answered around why it happens, who is being affected, and how doctors should handle the cases.
For example, one report from Veterans Affairs doctors describes a 71-year-old man who saw his COVID-19 symptoms quickly clear up after two days of taking the drug. But four days after finishing the full course of Paxlovid, his symptoms — including a runny nose and sore throat — returned for a few more days.
The Centers for Disease Control and Prevention has been consulting with the National Institutes of Health over potential data sources that can be used to study the cases, a CDC spokesperson said in a statement. No NIH studies are underway yet, the NIH said in a statement, though federal scientists are “actively discussing” ways to investigate the phenomenon.
Pfizer executives say reports of COVID-19 symptoms and positive tests returning after taking their drug remain uncommon.
“We do surveillance of patients in very large databases. And we have access to more than 300,000 Paxlovid treated in one of the databases. We have reports of this happening in about 0.005% or less,” Dr. Mikael Dolsten, Pfizer’s chief scientific officer, told the company’s investors during an earnings call this week.
Around 2% of patients saw a rebound in Pfizer’s clinical trials of Paxlovid, the company’s executives pointed out, regardless of whether they got the drug or a placebo.
“It’s not really related to Paxlovid, but more to the individuals that then need to clear the virus. And it is a virus that can either reinfect patients or there can be reservoirs left in the patients,” Dolsten said.
FDA says “no evidence” taking more Paxlovid helps
The Food and Drug Administration says that there is “no evidence” that taking more pills of Paxlovid will help patients who see a resurgence of the disease.
The FDA’s statement came a day after top executives at Pfizer said patients who have symptoms come back after finishing off the five-day treatment could simply start a new round of the pills.
“It could be that in some cases, there is a rebound. That was why the label speaks about the second treatment that can be given,” Pfizer’s CEO Albert Bourla told investors.
Writing in NEJM Journal Watch, Harvard Medical School’s Dr. Paul Sax said doctors have also been told by Pfizer and the FDA that they can prescribe another round of pills – treating the apparent rebound like they would a reinfection.
“In other words, the within-5-day symptom clock starts over with the relapse. This would be justified clinically for our highest-risk patients (severely immunocompromised, medically fragile, or with severe recurrent symptoms), and favored over other outpatient treatments (all of which have logistical or efficacy issues) until we know more,” Sax wrote on Wednesday.
A spokesperson for Pfizer declined to comment “on conversations between medical professionals,” but said that “there are no limitations” in the FDA’s emergency use authorization for treating “subsequent COVID-19 infections” in eligible patients.
However, doctors caution that even the theoretical argument for an additional course remains tenuous — and that a second round of pills is not without its downsides.
While Pfizer and the FDA say they have not spotted any signs of resistance to Paxlovid in rebound cases so far, experts warn that increased use of the drug could increase the risk of the virus evolving resistance.
In addition, many patients taking Paxlovid must put off taking other needed medications that can interact with the treatment.
“We have no data to support that a second course really is a benefit. Anecdotally, most people simply get better. We have a lot of theoretical reasons why maybe that second course isn’t needed,” says Dr. Roy Gulick, chief of the division of infectious diseases at Weill Cornell Medicine.
Pfizer’s authorization for the drug is based on data from a clinical trial that was done during the Delta variant, Gulick points out, studying Paxlovid in unvaccinated people at high risk of severe disease.
The FDA says that in the clinical trial, most patients who began to test positive again after finishing their initial round of pills were asymptomatic, and were not more likely to be hospitalized or die from the disease. Late last month, Pfizer disclosed that another recent trial looking to see if its drug could prevent infections after exposure failed to meet statistical significance.
“We are extrapolating in both those senses because many of the people at high risk for progression of COVID, of course, are fully vaccinated and fully boosted. So does Paxlovid really provide additional benefits in that group, particularly in the time of Omicron and the subvariants? We don’t know the answer to that,” added Gulick.
Speaking on Friday, Dr. John Farley, the FDA’s top official overseeing drugs, underscored that Paxlovid was authorized with the aim of reducing the risk of severe disease, not necessarily “on the basis of symptom improvement.”
“These reports do not change the conclusions from the Paxlovid clinical trial, which demonstrated a marked reduction in hospitalization and death, nor is there data at this time that would support a general change in clinical management,” Farley said.
Gulick, who serves as a co-chair of the NIH’s influential COVID-19 Treatment Guidelines panel, declined to comment on when or whether the group would issue guidance on how providers should handle these cases.
“I will say the guidelines are responsive to what’s being talked about out there. And so clinical controversies, the guidelines certainly wants to help with,” said Gulick, adding that “the guidelines review data and make data-driven decisions. So data are important to help inform this.”
For now, Gulick acknowledged that providers — including himself — have been in the “uncomfortable” position of trying to help counsel patients through deciding whether to take another round of the drug amid a flood of unanswered questions and anecdotes.
“In the end, it was shared decision-making, and we elected not to use a second course of Paxlovid,” Gulick recalled of a recent patient he treated with Paxlovid who then saw their symptoms return.
The patient, who was vaccinated and boosted, was over 65 — the age group at highest risk of severe disease — and had several underlying conditions. Continuing Paxlovid would have meant the person would need to keep delaying a needed cholesterol medication, Gulick said.
“The patient fully recovered, a happy person. That’s about as anecdotal as it gets,” said Gulick.







