This article was republished with permission from WTOP’s news partners at Maryland Matters. Sign up for Maryland Matters’ free email subscription today.
This content was republished with permission from WTOP’s news partners at Maryland Matters. Sign up for Maryland Matters’ free email subscription today.
Maryland state officials are pushing a statewide informational campaign to ensure that Marylanders who are still eligible for Medicaid do not lose out on coverage now that the public health emergency for COVID-19 has come to an end.
“While we remain committed to fighting COVID-19, we recognize that this milestone brings change. This includes the return of Medicaid renewal,” said Secretary of Health Laura Herrera Scott at a Thursday press conference announcing the state’s informational campaign.
Medicaid is a federal program for low-income individuals and families to receive health insurance funded by federal and state dollars.
Pre-pandemic, Medicaid recipients had to re-enroll annually to redetermine eligibility. But over the COVID pandemic years, states were prohibited from rolling people off the program even if some no longer qualified so that people could maintain coverage during the global health crisis.
Due to the pressing COVID pandemic, Maryland’s Medicaid enrollment increased by some 375,000 participants since February 2020, according to data from the state Department of Health, meaning that thousands of people participating in Medicare have never been through a re-enrollment period, while others have not been through a re-enrollment period for several years.
The issue of people unnecessarily falling off of Medicaid coverage is referred to as “Medicaid unwinding,” and Maryland health officials want to make one thing clear:
“Maryland Medicaid renewal is not automatic this year,” according to a flyer adverting the so-called “Medicaid Check-in” campaign.

Secretary of Human Services Rafael López said that Marylanders need to make sure their contact information and mailing addresses are updated with the state to make sure that they receive renewal notices and can complete the necessary paperwork on time.
“If you receive Medicaid benefits, and do not complete renewal, or provide incomplete information, your coverage may be terminated. When you lose Medicaid coverage due to a failed renewal, you may be left without access to necessary medical care, medications and other necessary treatments,” Lopez said Thursday.
The Thursday press conference included Spanish and American Sign Language translations. The informational campaign will include digital billboards, television and radio commercials, social media advertisements, text messages and mail notifications.
Phases of reevaluations
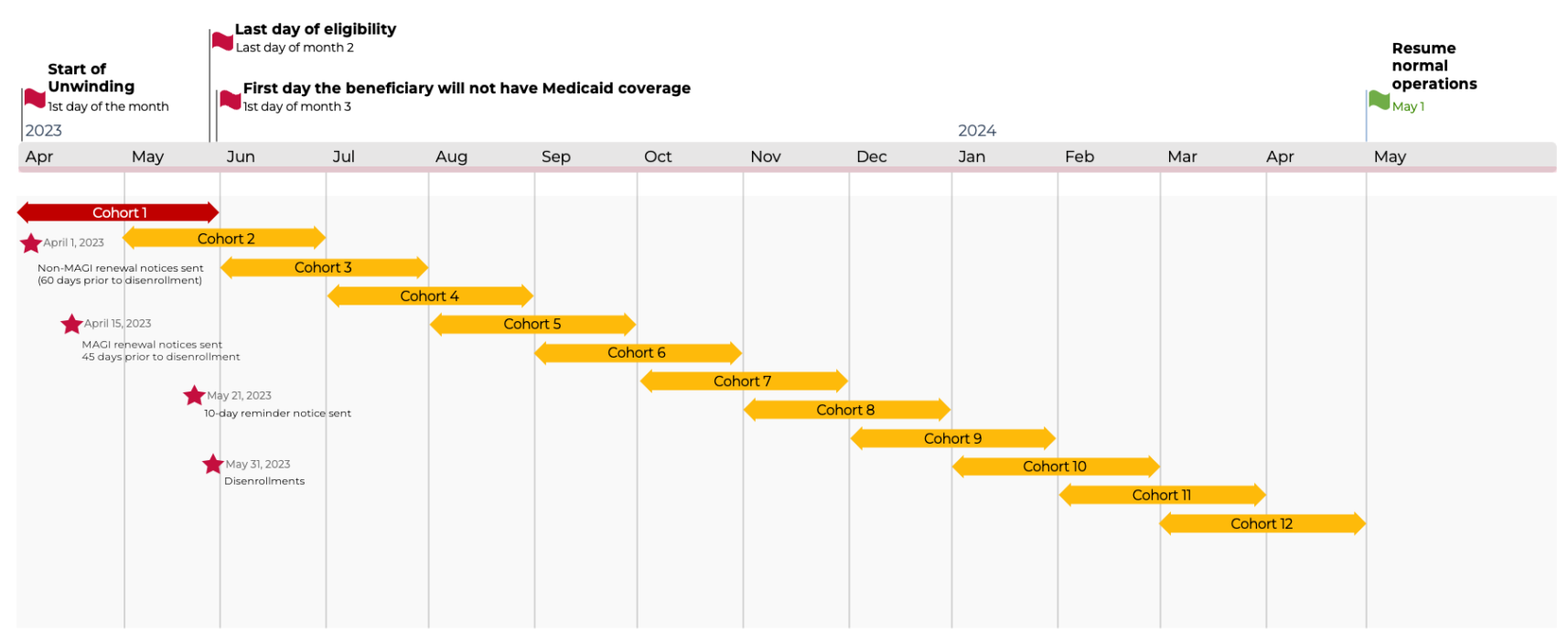
Due to the nearly 1.8 million Marylanders who will need to re-enroll in Medicaid this year, the state Department of Health decided to issue reevaluations and any subsequent disenrollments in monthly phases. These reevaluations will be finalized by May 2024.
Each “cohort” of Marylanders will be able to apply for renewal when they receive a notice from the Maryland Health Connection or the Department of Human Services. From then, they will have 45 days to renew. There will be twelve cohorts in total.
Those who qualify but do not re-enroll will be at risk of losing coverage. Those who get rolled off of Medicaid due to ineligibility are recommended to find an affordable health care coverage through the Maryland Health Connection.
Herrera Scott said Thursday that it’s difficult to gauge how many Marylanders are at risk of losing Medicaid in the unwinding period,
But state health officials will look at data as it comes in monthly to make adjustments to their messaging as needed, according to Deputy Secretary Ryan Moran, the health and healthcare finance and Medicaid director at the department.
“We’ll be using that data and developing more robust reporting than what’s available right now as we move forward,” Moran told Maryland Matters.
The current state data shows that 54,856 Medicaid beneficiaries have renewed and retained coverage as of April 31, though this is not the final count for the first cohort of Medicaid reconsiderations.
The data reports that there are 320 renewals that have not yet been completed and will have until May 31st to complete their renewal. Meanwhile, there have been 387 people who were determined ineligible, meaning they will not have access to Medicaid coverage starting June 1.
According to non-profit health-policy research and polling organization KFF, Medicaid unwinding plans and unenrollment periods will vary across the United States.
Maryland will officially begin to roll-off the first cohort from Medicaid in June, Moran from the Department of Health said. That’s also the case for 20 other states and Washington, D.C., according to KFF’s report.
There are five states that started rolling people off as early as April: Arkansas, Arizona, Idaho, New Hampshire and South Dakota.
For example, more than 40,000 Arkansans lost Medicaid coverage due to not updating their information with the state, according to the Arkansas Advocate.
At the start of May, 14 other states began their disenrollment periods, including Maryland’s neighboring states Pennsylvania, Virginia and West Virginia. Delaware will begin disenrolling people from Medicaid in July, according to KFF.







