


Despite current recommendations, 22% of women 35 to 44 years old have never gotten a mammogram and have no plans of getting one, according to a national survey by Orlando Health.
Women of average risk should begin yearly breast cancer screening mammograms at age 40, according to updated guidelines from the National Comprehensive Cancer Network (NCCN), which also recommends that women assess their risk of developing breast cancer about age 25.
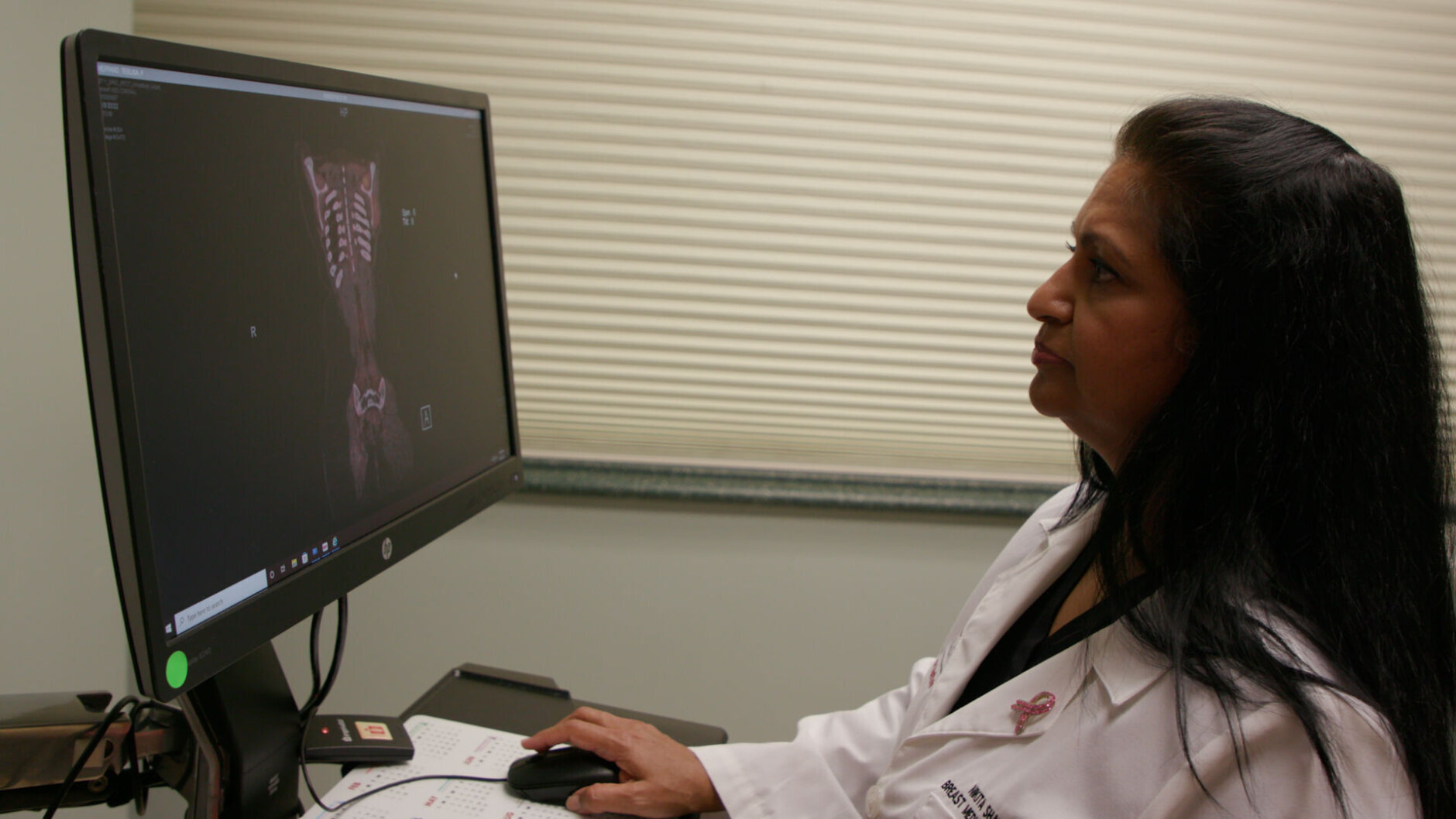
“That’s important because as an individual person, you want to know what is your risk of developing breast cancer. What are the things you need to be doing differently? And at what age?” said Dr. Nikita Shah, medical oncology team leader for the Breast Care Center at the Orlando Health Cancer Institute.
Risk assessments, typically done either by primary care physicians or a gynecologist, take into consideration things, such as family history, dense breast tissue and abnormal biopsy results.
“Another big thing (from the survey) is that only about 43% of women know their family history of not just breast cancer, but cancers,” Shah said.
Shah emphasized that family history from fathers also matters when assessing breast cancer risk.
“Family history matters from either side of the family because we get half our genes from our mother and half the gene from the father,” she said. “And it’s not just breast cancer history. It’s also history of other cancers like colon cancer, prostate cancer, ovarian cancer, pancreatic cancer.”
The mammogram guidelines have become more liberal, according to Shah, because a patient’s family might be small or they might not have contact with their families. Guidelines also suggest whether someone should undergo testing for genetic mutations.
“If we find that somebody has a BRCA1 or BRCA2 mutation, they may be recommended prophylactic mastectomy even before they develop cancer because we want to do things to prevent them from actually going through a cancer diagnosis and the treatment of that,” Shah said.
People who inherit harmful variants in one of these genes have increased risks of several cancers—most notably breast and ovarian cancer, but also several additional types of cancer, the National Cancer Institute said.
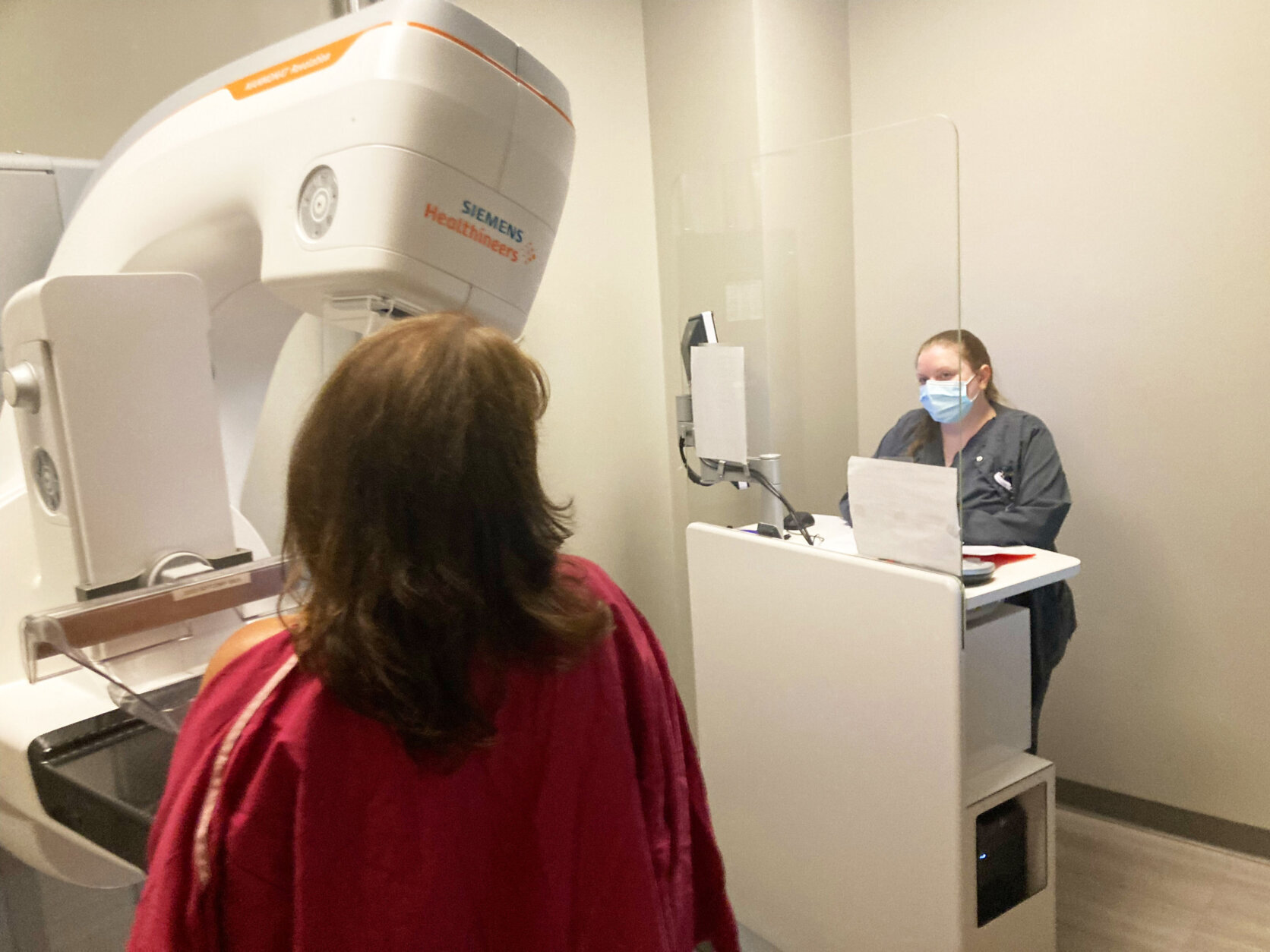
Mammograms can catch cancer very early when the cure rate is more than 95% versus a cancerous tumor found in later stages when it might have spread, and the likelihood of remissions is significantly higher.
“Please go get a mammogram,” Shah said. “There is no reason why you shouldn’t if you are 40 and above.”








