This content is sponsored by Johns Hopkins Medicine.
Conventional photon radiation is very effective at treating many cancers but can pose a particular risk for some patients with brain and spinal cord tumors.
With conventional photon radiation treatment, the powerful doses required to destroy tumor cells — standard for many cancers of the brain and spinal cord — can damage the surrounding healthy tissue, not just the tumors it is targeting. The resulting side effects can be significant if the tumors are right up against critical structures that are involved in neurocognitive function — vision and hearing, for example.
Enter the Johns Hopkins Proton Therapy Center, located at Sibley Memorial Hospital, which offers precision treatment for adult and pediatric patients, including for tumors of the brain and spinal cord.
Traditional photon radiation treatment uses powerful X-rays to attack cancer cells, but photon radiation doesn’t stop traveling once it enters the body. That means it requires sophisticated treatment planning to minimize its effects on healthy tissue.
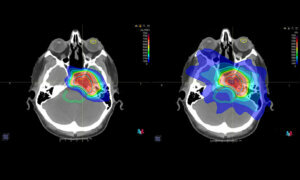
Proton therapy, in contrast, takes advantage of a unique characteristic of high energy heavy particle beams and how they deposit radiation as they move through the body: Virtually all their energy is deposited within the tumor, with a minimal amount exiting and being absorbed by surrounding tissues. The precision of proton therapy helps avoid unnecessary damage to adjacent healthy cells, decreasing the risk of secondary cancers.
The 80,000-square-foot center’s physicians use sophisticated image guidance and “pencil beam” scanning technology, the most advanced form of proton therapy delivery, to precisely target tumors and deliver higher radiation doses to cancer cells while sparing nearby vital organs and normal tissues.
The facility, which has three large mechanical arms called gantries that can move the proton beam 360 degrees around the patient, is staffed with experts from the Johns Hopkins Kimmel Cancer Center.
“We use the latest proton technology to help reduce side effects that occur both during and after treatment in cases where tumors grow in critical areas,” says Christina Tsien, M.D., medical director of the proton center and a leading expert in the treatment of brain tumors.
She says proton therapy may be suitable for brain and spinal cord radiation in cancers such as:
· Chordomas and chondrosarcomas
· Skull base meningiomas
· Diffuse gliomas
· Pediatric and adult medulloblastoma, a cancer that starts in the lower back part of the brain and is the most common pediatric brain cancer
· Ependymomas, a rare tumor that can occur in the brain and spinal cord
The proton center collaborates with Children’s National Hospital, expanding an earlier partnership between the two institutions that helped establish Sibley’s pediatric radiation oncology program. “We want our pediatric patients to maintain a long, healthy life,” Tsien says. “Our focus is on trying to reduce treatment-related complications and providing our pediatric patients with the most state-of-the-art technologies.”
Part of Tsien’s research focuses on the safety and efficacy of using proton radiation to treat brain tumors that have progressed following previous treatments.
She says this approach may improve tumor control and avoid neurologic symptoms, which can range from headaches and seizures to loss of balance and changes in vision.
Her research on glioblastoma — the most aggressive form of brain cancer — dovetails well with her work at the proton center, she says. “My research has been on using advanced imaging to help understand biologically where the most active part of the tumor is,” she says. “Being able to use this information to target the most aggressive areas of the tumor with proton therapy is of great interest.”




